Chloroquine and Hydroxychloroquine (HCQ) should only be used if they are prescribed by a physician, the Ministry of Health said in a statement.
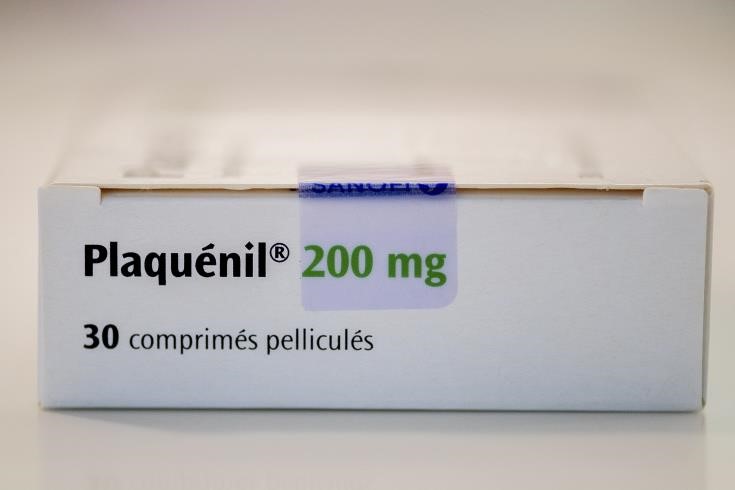
Citing the European Medicines Agency, (EMA) the Ministry said the two medicines are currently authorised for malaria and certain autoimmune diseases. They are being investigated worldwide for their potential to treat coronavirus disease (COVID-19). However, efficacy in treating COVID-19 is yet to be shown in studies.
It is very important that patients and healthcare professionals only use chloroquine and hydroxychloroquine for their authorised uses or as part of clinical trials or national emergency use programmes for the treatment of COVID-19, the press release said
Both chloroquine and hydroxychloroquine can have serious side effects, especially at high doses or when combined with other medicines. They must not be used without a prescription and without supervision by a doctor; prescriptions should not be given outside their authorised uses except in the setting of a clinical trial or nationally agreed protocols.
Large clinical trials are under way to generate the robust data needed to establish the efficacy and safety of chloroquine and hydroxychloroquine in the treatment of COVID-19, the Ministry said, adding that the European Medicines Agency EMA welcomes these trials, which will enable authorities to give reliable advice based on solid evidence to healthcare professionals and patients.
Considering the urgency and the pressure healthcare systems face to save lives during the COVID-19 pandemic, some countries, including the USA and France, have put strict protocols in place to allow the experimental use of these two medicines, for example, in patients with severe forms of COVID-19.
It further added that Chloroquine and hydroxychloroquine are vital medicines for patients with autoimmune conditions such as lupus. It is important that such patients are still able to obtain them and do not face shortages caused by stockpiling or use outside the authorised indications. In some countries, prescribing of the medicines has been restricted to reduce the risk of shortages.
Patients should only use chloroquine or hydroxychloroquine if they have been prescribed for them and a doctor is supervising their treatment.
Chloroquine and hydroxychloroquine should continue to be used in chronic conditions. In order to prevent unnecessary strain on supply chains, patients should only receive their usual supply of medicines. Healthcare professionals should not write prescriptions that cover more than the usual duration.
Meanwhile, EMA said that supporting the rapid development and approval of effective and safe treatments for and vaccines against COVID-19 is the organisation’s top priority to help save lives during the pandemic. Over recent weeks and months, the Agency has engaged with many developers of therapeutic medicines and there are a number of developments underway. However, at this point, on the basis of the preliminary data presented to the Agency, no medicine has yet demonstrated efficacy in treating COVID-19.
EMA’s COVID-19 response team has been in contact with developers of around 40 therapeutic medicines, allowing better understanding of potential treatments.
Among the potential treatments for COVID-19 that are undergoing clinical trials to assess their safety and efficacy against the disease are:
- lopinavir/ritonavir (currently authorised as an anti-HIV medicine)
- remdesivir (investigational)
- chloroquine and hydroxychloroquine (currently authorised at national level as treatments against malaria and certain autoimmune diseases such as rheumatoid arthritis)
- systemic interferons and in particular interferon beta (currently authorised to treat diseases such as multiple sclerosis)
- monoclonal antibodies with activity against components of the immune system
It further welcomed the launch of large clinical trials as they are necessary to generate the robust data needed to establish evidence for which medicines do work and thus to give appropriate advice to healthcare professionals and patients and enable regulatory decision-making, as advised by EMA’s human medicines committee (CHMP).
The Agency has also had discussions with developers of a dozen potential COVID-19 vaccines. Two vaccines have already entered phase I clinical trials, which are the first trials needed and are carried out in healthy volunteers. In general, timelines for the development of medicinal products are difficult to predict.
Based on the information currently available and past experience with vaccine development timeframes, EMA estimates that it might take at least one year before a vaccine against COVID-19 is ready for approval and available in sufficient quantities to enable widespread use. Adequate supply of doses to meet the needs of all EU countries has to be proactively forecast.
EMA’s response team will continue to interact with developers of potential therapeutics or vaccines against COVID-19. The aim is to provide advice on regulatory requirements so that any promising medicinal product can be made available as rapidly as possible to patients, initially in the clinical trial setting and then, once authorised, on the market.
Source: CNA